When it comes to managing diabetes, particularly Type 1 diabetes, two major treatment options come into play: insulin therapy and pancreas transplantation. Both offer benefits but also present their own challenges. Deciding which is better, insulin or pancreas transplant, depends on several factors, including a patient’s specific condition, lifestyle, and long-term health goals. This blog will explore the pros and cons of Pancreas Transplant vs. Insulin and help you understand their differences from both a medical and practical standpoint.
What is a Pancreas Transplant?
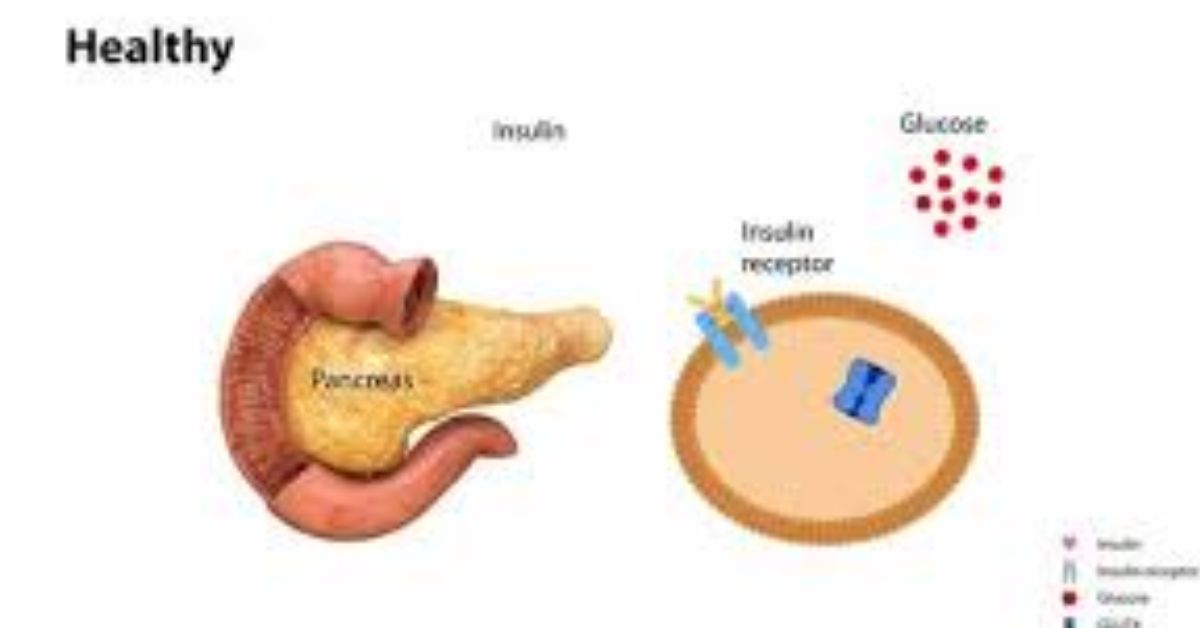
A is a surgical procedure where a healthy pancreas from a deceased donor is transplanted into the recipient’s body. The purpose of the transplant is to restore the body’s ability to produce insulin, a hormone that regulates blood sugar levels. For patients with Type 1 diabetes, where the immune system attacks the insulin-producing beta cells of the pancreas, a pancreas transplant offers a potential cure for the condition.
In many cases, a pancreas transplant is performed in conjunction with a kidney transplant for those who also have kidney failure as a result of diabetes. However, it can be performed as a standalone procedure for patients who have severe, insulin-dependent diabetes and struggle with maintaining healthy blood sugar levels despite insulin therapy.
What is Insulin Therapy?
Insulin therapy is the standard treatment for individuals with Type 1 and Type 2 diabetes. It involves injecting insulin into the body to help regulate blood sugar levels. The insulin can be administered through daily injections, an insulin pen, or an insulin pump. The goal is to mimic the body’s natural insulin production and allow the individual to maintain normal blood sugar levels, reducing the risk of complications like heart disease, nerve damage, and kidney failure.
Pancreas Transplant vs. Insulin: Key Differences
Mechanism of Action
- Pancreas Transplant: A pancreas transplant provides a new, fully functional pancreas that produces insulin naturally, much like a healthy pancreas in someone without diabetes. Once the transplant is successful, the patient may no longer need insulin therapy as their new pancreas can regulate blood sugar levels on its own.
- Insulin Therapy: Insulin therapy requires continuous monitoring and management of blood sugar levels. The patient must inject insulin or use a pump throughout the day to ensure they have the right amount of insulin in their system. Unlike the natural pancreas, insulin injections do not perfectly mimic the body’s hormone production.
Effectiveness in Diabetes Management
- Pancreas Transplant: A successful pancreas transplant can offer diabetes remission, meaning the patient may no longer need to take insulin or monitor their blood sugar as closely. In the best-case scenario, the transplant leads to a near-normal quality of life with better overall blood sugar control and fewer long-term complications from diabetes.
- Insulin Therapy: While insulin therapy helps manage blood sugar levels effectively, it does not cure diabetes. It is a lifelong treatment that requires constant adjustment and management. Even with modern technology such as insulin pumps and continuous glucose monitors, maintaining perfect blood sugar control can be challenging.
Eligibility and Availability
- Pancreas Transplant: Pancreas transplantation is not suitable for every diabetic patient. It is generally considered for patients with Type 1 diabetes who also have kidney disease or for those with extremely severe and hard-to-control diabetes. The process involves waiting for a suitable donor organ, and the procedure itself carries significant risks. As a result, pancreas transplants are less common than insulin therapy.
- Insulin Therapy: Insulin therapy is widely available to anyone with diabetes. It is the standard of care for people with Type 1 diabetes and is also used by some people with Type 2 diabetes. Since insulin injections are simple and low-risk, they are accessible to nearly everyone with diabetes.
Risks and Side Effects
- Pancreas Transplant: While pancreas transplantation offers the potential for diabetes remission, it also comes with several risks. The procedure is major surgery and carries the risk of complications such as organ rejection, infection, blood clots, and other transplant-related issues. Furthermore, the patient must take immunosuppressive medications to prevent rejection, which come with their own set of side effects, such as a weakened immune system, increased risk of infections, and long-term side effects like kidney damage.
- Insulin Therapy: Insulin therapy is relatively safe when properly managed, but it is not without its risks. Patients may experience hypoglycemia (low blood sugar) if too much insulin is taken or if meals are skipped. Additionally, poor insulin management over time can lead to complications such as weight gain, insulin resistance, and a higher risk of cardiovascular disease.
Lifestyle Impact
- Pancreas Transplant: After a pancreas transplant, patients may experience significant improvements in their lifestyle. If the transplant is successful, they can avoid the daily routine of insulin injections and blood sugar monitoring. This can greatly improve their quality of life, reducing the stress and burden of diabetes management. However, the patient must commit to a lifetime of anti-rejection medications, which can have side effects and may impact long-term health.
- Insulin Therapy: Insulin therapy allows for flexibility in managing diabetes, but it also requires ongoing effort. Patients need to monitor their blood sugar levels regularly, calculate carbohydrate intake, and adjust insulin doses as needed. While advancements in insulin delivery methods have made this process easier, it still requires a significant commitment to self-management.
Cost and Accessibility
- Pancreas Transplant: Pancreas transplantation is an expensive and complex procedure. The costs can include not only the surgery itself but also post-operative care, hospital stays, and lifelong immunosuppressive medications. Furthermore, the waiting list for donor organs can be long, and there is no guarantee of a successful transplant.
- Insulin Therapy: Insulin therapy is generally more affordable and widely accessible than pancreas transplantation. The costs vary depending on the type of insulin and delivery method (e.g., insulin pumps, pens, or syringes), but it is generally a lower-cost option compared to the lifelong expenses associated with a transplant.
Long-Term Outlook
- Pancreas Transplant: A successful pancreas transplant can provide long-term benefits, including diabetes remission and a reduction in the risk of complications associated with diabetes. However, the transplant’s success is not guaranteed, and some patients may experience rejection or other complications. The long-term outcome also depends on the patient’s adherence to immunosuppressive medication.
- Insulin Therapy: With proper management, insulin therapy can help prevent long-term complications of diabetes, such as neuropathy, retinopathy, and kidney disease. However, it does not eliminate the risk of these complications. Patients must remain vigilant and manage their blood sugar levels consistently over time.
Which is Better: Pancreas Transplant or Insulin Therapy?
The decision between a pancreas transplant and insulin therapy largely depends on the individual’s specific health needs, lifestyle, and preferences. For some patients, particularly those with severe complications from diabetes such as kidney failure, a pancreas transplant may offer a better solution. It can provide the potential for a cure and eliminate the need for insulin injections. However, the carries significant risks and requires a lifelong commitment to immunosuppressive medications.
On the other hand, insulin therapy is a well-established, widely available, and more accessible option for managing diabetes. While it may not cure diabetes, it can effectively control blood sugar levels and prevent complications when managed properly. Insulin therapy is generally less invasive and does not carry the same risks as a transplant.
Conclusion
Both pancreas transplants and insulin therapy have their advantages and disadvantages. Choosing the right treatment depends on individual circumstances, including the severity of diabetes, overall health, access to medical care, and the patient’s willingness to undergo surgery and take immunosuppressive medications. For most people with diabetes, insulin therapy remains the standard treatment, while pancreas transplantation is considered for those with severe, life-threatening complications or those who seek a potential cure for their condition.
Ultimately, the goal is to manage blood sugar levels effectively, reduce the risk of complications, and improve overall quality of life. It’s important for patients to consult with their healthcare providers to determine the best treatment plan based on their unique needs and circumstances.